Medical billing errors are more common than you might think, and they can wreak havoc on both healthcare providers and patients alike. Let’s be honest—dealing with claim denials and insurance headaches is no fun for anyone. As a provider, it’s not just frustrating to watch claims get rejected, but it can also seriously impact your bottom line. In fact, did you know that a huge percentage of medical bills contain errors?
It’s a big issue, but here’s the good news: addressing these errors promptly can totally turn around a practice’s revenue cycle. Now, with the rise of AI in medical billing, we’re seeing a huge shift. AI is stepping in to reduce these errors significantly, making billing practices more accurate and efficient than ever. But here’s the real question: how do we fix these errors? Let’s take a closer look at the most common medical billing errors, why they happen, and most importantly—how to fix them once and for all! Ready? Okay let’s look for these errors, then.
Why Do These Errors Happen?
So, the first question is; why do these errors happen? Medical billing errors happen for a variety of reasons, and while they can feel frustrating, they’re often the result of human mistakes, complex systems, and outdated practices. Medical billing is a high-stakes, detail-heavy process, where even the smallest mistake—whether it’s a typo or a missed insurance verification—can lead to claim denials and financial setbacks. The fast-paced nature of healthcare combined with increasing insurance requirements makes it easy for these errors to slip through the cracks. However, addressing these issues head-on can save time, reduce stress, and ensure that you’re getting reimbursed properly.
The Cause of These Errors?
- Human oversight: Inaccurate patient information or missed steps in the coding process.
- Complexity: Healthcare systems and insurance policies are constantly evolving, making it difficult to keep up.
- Lack of training: Inadequate knowledge or training in billing and coding can lead to mistakes.
- Outdated systems: Using old software or manual methods can increase the chances of errors slipping by.
Top 10 Medical Billing Errors and Fixes
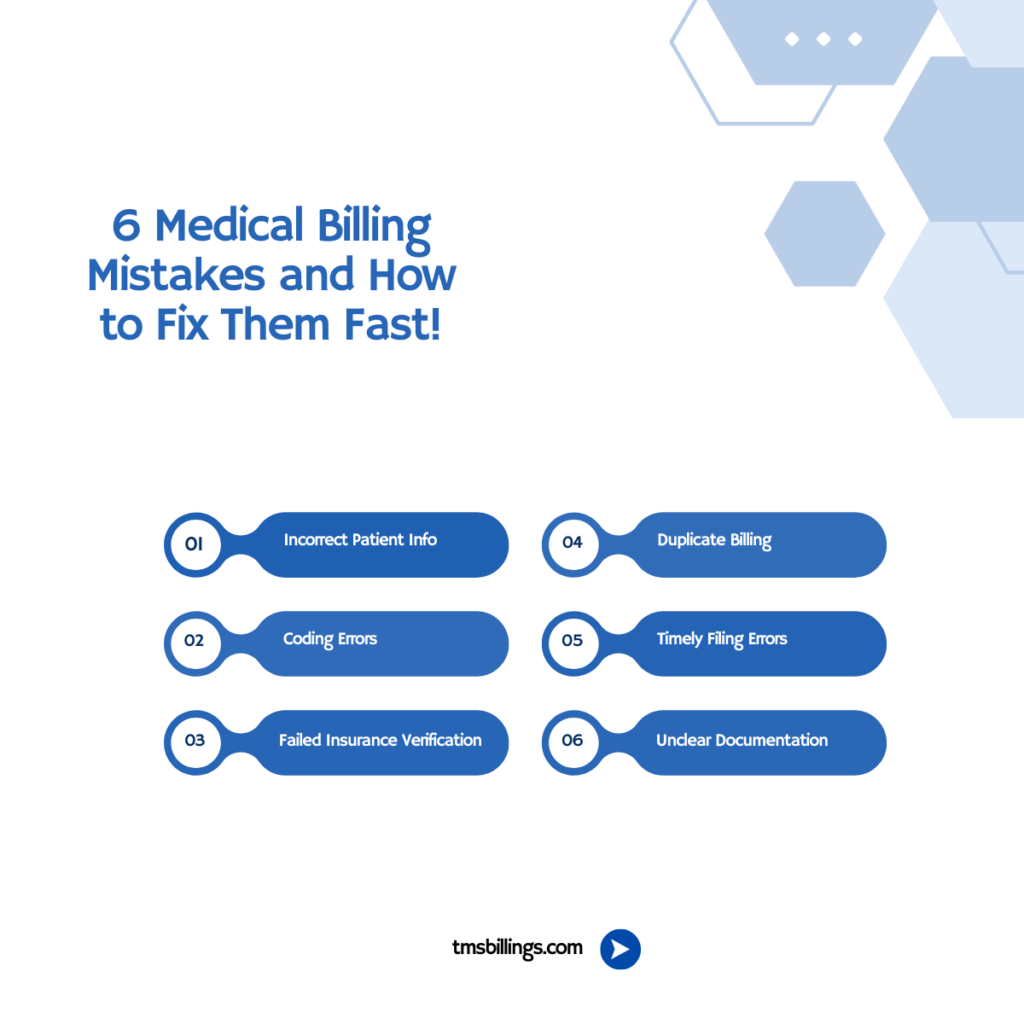
Medical billing errors can be costly and time-consuming, but identifying and fixing them is key to smoother operations. Here’s a quick rundown of the 10 most common billing errors and how to correct them to keep your revenue cycle on track.
i. Incorrect Patient Information
The first and most basic medical billing error involves inaccurate or incomplete patient information. This includes incorrect names, birthdates, insurance numbers, or addresses. If the insurance provider cannot match the patient to their correct policy, the claim gets rejected.
How to Correct This?
- Double-check all patient information before submitting claims.
- Ensure that updated and accurate information is entered into your system from the very beginning of the patient’s visit.
With medical billing and coding errors, ensuring that patient details match across the board is crucial to preventing denial of claims.
ii. Coding Errors in Medical Billing
Incorrect or incomplete coding is one of the most common medical billing errors. These errors occur when codes used in the claim don’t accurately reflect the services provided or the diagnosis made. This is where medical billing and coding errors and AI algorithms can make a big difference in improving accuracy.
How to Correct This?
- Use certified medical coders who are thoroughly trained.
- Regularly update coding practices to ensure compliance with the latest ICD-10, CPT, and HCPCS codes.
- AI-driven systems can also help reduce these errors by suggesting correct codes, especially with AI reduce coding errors technology.
iii. Failed Insurance Verification
Another frequent issue is failing to verify insurance coverage. Many medical bills get rejected because the provider didn’t confirm that the patient’s insurance was active or didn’t cover the specific procedure. If a claim is filed for an inactive insurance policy or a service not covered under the policy, the claim is denied.
How to Correct This?
- Implement a robust insurance verification process before services are rendered.
- Check the patient’s insurance coverage both at the time of scheduling and again on the day of the appointment.
It’s also worth considering working with a credentialing service provider like TMS Billings Credentialing Services. This ensures that all insurance plans are verified properly to avoid future denied claims.
iv. Incorrect or Missing Provider Information

Credit: mednetinc.com
Sometimes, medical bills get rejected because the provider’s details are incorrect. This can include missing or incorrect National Provider Identifier (NPI) numbers or provider tax ID numbers.
How to Correct This?
-
Keep your provider information up-to-date with all insurance carriers.
-
Regularly audit the information in your system to ensure that it’s accurate.
v. Duplicate Billing
Duplicate billing is another common medical billing error that happens when the same service is billed multiple times, either due to system errors or human oversight. This can lead to overpayments, delayed reimbursements, and claim denial.
How to Correct This?
- Implement a claim tracking system to check for duplicate submissions.
- Train staff to carefully review each claim before submission.
Using automated tools or AI-driven billing software can help you significantly reduce these kinds of errors by automatically flagging duplicates before they’re submitted to insurers.
vi. Misunderstanding of Insurance Policies
Sometimes providers make assumptions about what is covered by a patient’s insurance, leading to billing errors. Whether it’s assuming certain procedures are covered or failing to understand insurance coverage for specific treatments, mistakes happen often.
How to Correct This?
- Provide staff training on various insurance policies so they understand what is covered.
- Use AI systems to cross-check coverage before submitting claims.
By staying informed about insurance policies and regularly reviewing them, you can avoid submitting claims for services that are not covered.
vii. Unclear or Insufficient Documentation
Sometimes, a claim is rejected due to insufficient documentation to support the medical necessity of a service or procedure. Without clear notes from healthcare providers, insurance companies may deny claims for not meeting their medical necessity guidelines.
How to Correct This?
- Ensure all patient visits are thoroughly documented.
- Use checklists for each service to make sure documentation is complete and clear.
viii. Timely Filing Errors
Credit: outsourcestrategies.com
Each insurance company has its own policy for how long after a service they will accept claims. If a claim is submitted too late, it can get rejected due to timely filing errors. Providers must be aware of the timely filing guidelines for each payer to ensure they don’t miss out on reimbursement.
How to Correct This?
- Ensure claims are submitted promptly, ideally within 30 days of service.
- Set up reminders or automated systems to prevent delays.
ix. Incorrect or Unclear Claim Submission
Incorrect or incomplete submission of claims is a significant issue for many practices. Whether it’s submitting claims with the wrong codes, incorrect formats, or missing necessary documents, these kinds of errors can cause delays or denials.
How to Correct This?
- Implement a strict protocol for claim submission.
- Regularly audit claims before submission for accuracy.
- Using a trusted medical billing service, like TMS Billings Medical Billing Service, can ensure the claim submission process is efficient and accurate.
x. Failure to Appeal Denied Claims
After a claim denial, many practices fail to properly appeal the decision. This can be due to a lack of time, resources, or understanding of the appeal process. However, you can often recover a denied claim if the appeal is properly filed.
How to Correct This?
- Set up a dedicated team to handle denied claims and appeals.
- Understand why the claim was denied and address the issues when filing the appeal.
By staying on top of denied claims and appealing them when appropriate, you can maximize your practice’s revenue cycle.
FAQ’s
Here’s a look at the top FAQs to help you tackle medical billing errors and keep your practice on track.
What are the most common medical billing errors?
Coding mistakes, incorrect patient details, and insurance verification issues.
How can AI reduce medical billing errors?
AI automates coding and flags errors before submission, improving accuracy.
What percentage of medical bills have errors?
About 80% of medical bills contain errors.
How do I fix medical billing errors?
Double-check patient info, ensure proper coding, and appeal denials quickly.
Is medical billing errors and omissions insurance necessary?
Yes, it helps protect your practice from financial risks due to mistakes.
Ending Remarks
Fixing medical billing errors is key to getting paid on time and boosting your practice’s revenue. By tackling common issues like incorrect patient info, coding mistakes, and insurance verification, you can minimize errors and keep your cash flow steady. With AI-driven solutions and smart billing practices, your claims process can run smoother than ever.
Need help? Let TMS Billings streamline your billing, or check out TMS Credentialing Services to ensure your practice stays on track with insurers. Let’s make billing easier, together!