Medical coding looks straightforward—until you’re the one staring at a CPT code that suddenly feels like a secret puzzle. I’ve learned firsthand that one tiny slip, one misplaced modifier, or one missed detail can snowball into claim denials, delayed payments, compliance headaches, and revenue quietly leaking out of your practice. Whether you’re a provider, a practice manager, or a coder like me who’s spent far too many late nights double-checking claims, understanding the most common medical coding mistakes is one of the smartest ways to protect your cash flow and streamline your entire billing process. The best part? Most of these issues are totally preventable once you know what to look for and commit to strong, consistent coding practices.
So let’s walk through the 8 medical coding mistakes that could cost you—and more importantly, how I’ve learned to stop them before they sabotage your bottom line.
Using Outdated Code Sets
Medical codes evolve constantly. Each year, CPT, ICD-10-CM, and HCPCS release updates. If your team isn’t keeping up, you’re already losing money.
Outdated code sets create:
- Denied claims
- Compliance issues
- Incorrect reimbursements
- Tedious rework
Why it happens:
Many practices forget to update their coding software or overlook annual guideline changes.
Quick fix:
- Always install yearly coding updates
- Subscribe to update alerts from AMA or CMS
- Train staff consistently using reputable sources like the AMA CPT® updates
Upcoding and Downcoding—Both Can Hurt You

Credit: aapc.com
Upcoding may trigger audits. Downcoding leaves revenue on the table. Both are among the most common mistakes in medical coding across specialties.
Examples:
- Billing a higher E/M code when documentation doesn’t support it
- Using a low-level code even though the case required more complexity
Why it happens:
- Inconsistent documentation
- Misinterpretation of coding guidelines
- Fear of audits
Quick fix:
Match every CPT/ICD-10 code strictly to provider documentation. When in doubt, clarify—never assume.
Missing or Misusing Modifiers
Modifiers are powerful. They add clarity, justify services, and help support medical necessity. They’re also easy to mess up.
Coding mistakes involving modifiers include:
- Adding unnecessary modifiers
- Forgetting required modifiers
- Using modifier 25 incorrectly
- Using bilateral modifiers inconsistently
Why it matters:
Inaccurate modifier use causes immediate claim rejections—especially for procedures requiring precise bundling rules.
Pro tip:
Teach coders to check payer-specific modifier rules. Medicare and commercial insurers often differ.
Incorrect or Incomplete Documentation
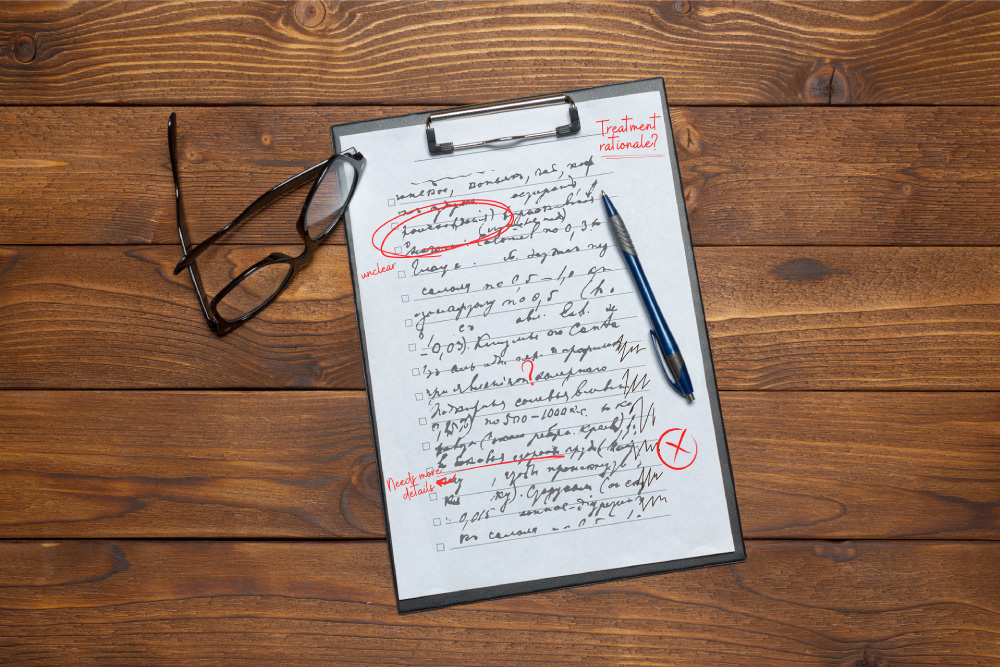
Credit: scribept.com
Even the best coder can’t guess what wasn’t documented. Documentation issues are one of the biggest reasons practices struggle with claim submission.
Common documentation errors:
- Missing signatures
- Incomplete procedure details
- No medical necessity justification
- Contradictory clinical notes
This leads to:
- Denials
- Downcoding
- Audit exposure
To strengthen documentation, consider partnering with specialists who align coding with strong clinical documentation improvement (CDI). Providers who work with expert medical coding teams see major reductions in denials and rework. You can explore how professional teams support accuracy with medical coding services.
Forgetting to Verify Payer-Specific Rules
Here’s a secret many coders don’t realize:
Different payers follow different rules—and these rules change fast.
Not verifying payer guidelines leads to:
- Incorrect bundling
- Wrong CPT coding
- Misused modifiers
- Frequent denials
Whether it’s Medicare, Blue Cross, or a niche payer, always cross-check coverage rules, NCCI edits, and documentation requirements. CMS publishes clear guidance on these rules.
Not Linking ICD-10 Codes to CPT Codes Properly
Credit: nethealth.com
This is one of the most costly coding mistakes—and one of the easiest to miss. If your diagnosis code doesn’t justify your procedure code, the claim automatically fails medical necessity checks.
Examples:
- Using a nonspecific diagnosis when a more precise code exists
- Missing multiple diagnosis codes needed to support a procedure
- Incorrect sequencing
Quick fix:
- Use the highest level of specificity
- Double-check LCD/NCD requirements for each CPT
- Train staff on correct linking logic
This alone can drastically reduce errors and speed up reimbursement.
Overlooking Bundled Services
Some services can (and should) be billed together, while others require unbundling. If your coders aren’t checking the National Correct Coding Initiative (NCCI) edits, you may be billing incorrectly without even realizing it.
Typical unbundling errors include:
- Billing separately for services included in a primary procedure
- Failure to use proper modifiers for allowed unbundling
- Billing multiple E/M codes without justification
These errors don’t just cause denials—they attract compliance audits.
Rushing Through the Billing Process

Credit: ccitraining.edu
Time pressure is a silent killer of accuracy. A rushed coder is a coder who makes mistakes.
When staff rush through the billing process, they may:
- Skip verification steps
- Miss key documentation
- Enter incorrect patient info
- Make typos in CPT or ICD-10
How to Reduce Errors:
- Implement double-review systems
- Automate repetitive tasks
- Use audit tools
- Outsource complex coding when overloaded
A strong revenue cycle management structure dramatically reduces these issues. Learn how optimized workflows prevent errors through revenue cycle management services.
Why Common Medical Coding Mistakes Are So Expensive
Every denied claim increases administrative cost. Every undercoded service decreases revenue. And every compliance risk can create long-term problems.
Mistakes affect:
- Reimbursement rates
- Provider compliance
- Patient satisfaction
- Operational efficiency
- Cash flow stability
Avoiding these traps isn’t optional—it’s essential.
How to Avoid Medical Coding Mistakes: Actionable Strategies

Credit: emmpeek.com
You can avoid the majority of errors by strengthening your workflow.
A. Train Your Team Regularly
Coding and billing rules change constantly. Consistent education reduces errors dramatically.
B. Use Technology Wisely
AI-driven coding tools, automated claim scrubbing, and RCM platforms help reduce manual errors.
C. Audit Your Claims Frequently
Regular internal audits identify risky patterns—and correct them early.
D. Improve Documentation Practices
Teach providers to document completely and clearly. Even brief clarifications save hours of rework.
E. Consider Outsourcing to Experts
Experienced teams catch common medical coding mistakes faster and ensure compliance across code sets and payer rules.
FAQ’s
Before we wrap up, here’s a quick look at the FAQs you’ve been asking most about medical coding mistakes.
What are the most common medical coding mistakes?
Using outdated codes, missing modifiers, incorrect documentation, and improper code linking are the top culprits.
How can I reduce coding errors in my practice?
Train your team, audit regularly, improve documentation, and use tech tools or expert coding partners.
Why do billing and coding errors cause so many denials?
Because payers require precise code accuracy—one mismatch triggers automatic rejection.
What mistakes do medical coders and billers make most often?
Unbundling errors, incorrect CPT coding, missing payer rules, and inconsistent documentation.
Is outsourcing medical coding worth it?
Yes—outsourcing helps reduce errors, speed up claim submission, and improve overall revenue flow.