Claim denials in medical billing—ugh, they can be such a pain, right? As a healthcare provider or someone handling medical billing, I’m sure you’ve felt the frustration of delayed payments, confused patients, and endless back-and-forth with insurance companies. It’s enough to make anyone want to pull their hair out! But here’s the thing: understanding why claim denials happen and how to prevent them is the secret to keeping your practice running smoothly and financially healthy.
Let’s take you through the common reasons behind claim denials in medical billing, share tips on how you can reduce them, and offer some best practices for managing denials like a pro. Trust me, knowing how to avoid those rejected claims will make your life a whole lot easier, and you’ll spend less time chasing down payments and more time focused on your patients. So, let’s get into it—together!
What is Claim Denial in Medical Billing?
Before we explore how to prevent claim denials, it’s essential to understand what a claim denial in medical billing is. A claim denial occurs when an insurance company refuses to pay for a medical service, procedure, or treatment provided to a patient. This can happen for a variety of reasons, including errors in documentation, issues with eligibility verification, or mistakes in medical coding.
Understanding the common causes of claim denials can help you avoid these mistakes and ensure that your claims are paid on time.
Common Reasons for Claim Denials in Medical Billing
Credit: acerhealth.com
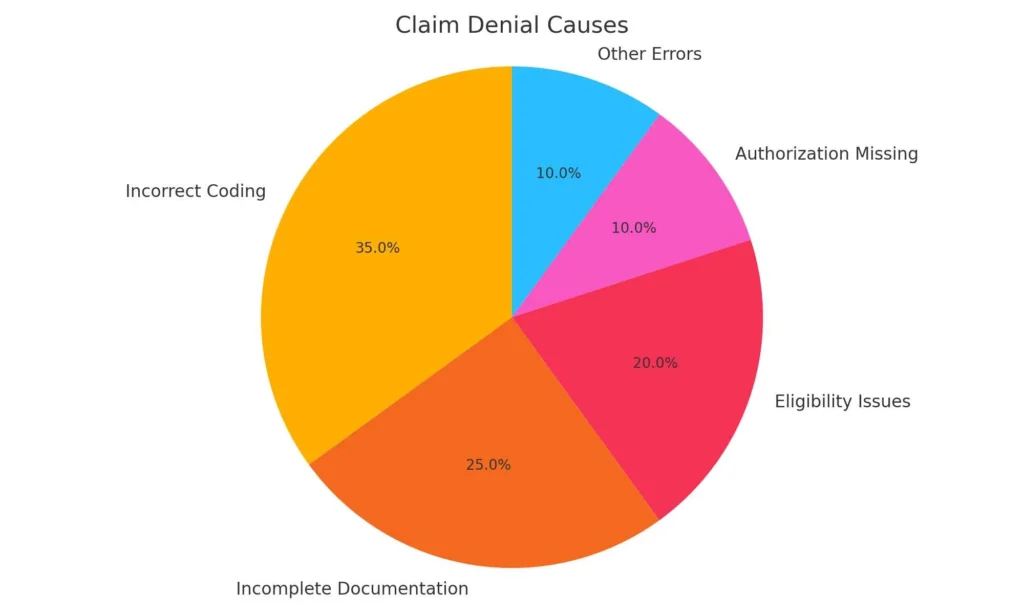
Medical billing is a detailed and complex process. Claims can be denied for many reasons, and identifying these reasons is the first step toward reducing claim denials. Here are some of the most common causes of claim denials:
A. Eligibility Verification Issues
- One of the most frequent reasons for claim denials in medical billing is incorrect or incomplete eligibility verification. If a patient’s insurance coverage details are not up to date or accurate, the claim will be denied.
- Solution: Ensure that eligibility verification is done before providing services. This can be done using software tools or contacting the insurance company directly to verify the patient’s coverage status.
B. Coding Errors
- Medical coding is a critical part of the billing process. If there are errors in the codes used to describe the services rendered, the insurance company will reject the claim. Coding and medical claim denials often occur when codes do not match the procedures or diagnoses.
- Solution: Work with experienced medical coders to ensure that all codes are accurate and reflect the services provided. If you’re looking for professional medical coding services, check out TMS Billing’s Medical Coding Services for expert assistance.
C. Prior Authorization Problems
- Some medical services require prior authorization from the insurance company before they can be provided. If this step is missed, the claim will be denied.
- Solution: Always check whether a service requires prior authorization before it’s delivered. This can be easily handled by establishing clear communication between the healthcare provider and insurance companies.
D. Inaccurate or Missing Information
- Claims may be denied when the information provided is incomplete or incorrect. This includes patient details, provider information, and service dates.
- Solution: Ensure that all patient details are correct and complete, including insurance policy numbers, service dates, and diagnosis codes. Double-checking this information can save a lot of time and prevent claim rejections.
E. Coding and Medical Claim Denials
- Some insurance companies may reject claims due to discrepancies in how the medical codes are used. For example, if the procedure code doesn’t align with the diagnosis code, the insurance company may consider it unsubstantiated.
- Solution: Proper training and communication between the medical billing and coding teams can help reduce these types of denials.
F. Lack of Medical Necessity
- Insurance companies will only pay for services that are deemed medically necessary. If the insurance company believes the treatment or procedure is not required, the claim will be denied.
- Solution: Ensure that the patient’s diagnosis clearly justifies the medical treatment provided, and include supporting documentation when submitting claims.
How to Reduce Claim Denials in Medical Billing
Credit: collaboratemd.com
Reducing claim denials in medical billing isn’t something that happens overnight. It requires a combination of strategies, training, and communication to minimize mistakes. Below are several best practices to reduce claim denials:
i. Effective Denials Management
- A proactive approach to denials management can significantly reduce the number of denied claims. Establish a system for monitoring and reviewing claims that are denied, and identify patterns or recurring issues.
- Solution: Use denial management tools to track and analyze the reasons behind claim rejections. Address recurring issues and take steps to prevent future denials.
ii. Improve Eligibility Verification
- One of the easiest ways to avoid claim denials is by verifying patient eligibility before providing services. Make sure all patient insurance information is accurate and up-to-date before treatment begins.
- Solution: Use real-time eligibility verification systems to streamline this process and reduce errors. Many medical billing services, such as TMS Billing’s Medical Billing Service, offer these solutions to ensure smooth and efficient verification.
iii. Ensure Accurate Medical Coding
- Medical coding is at the heart of the billing process, and accurate coding is essential to reduce medical billing claim denials. This means using the correct codes for diagnoses, procedures, and services rendered.
- Solution: Work with trained medical coders who stay updated with the latest coding standards and procedures.
iv. Utilize Prior Authorization
- For services that require prior authorization, make sure to get approval before the patient undergoes treatment. Failing to obtain prior authorization can lead to a denied claim.
- Solution: Develop a process that ensures all services requiring prior authorization are identified early and approved before treatment. This can save your practice time and money.
v. Stay Informed About Payer Requirements
- Insurance companies have different policies and guidelines, and keeping up with their requirements can prevent claims from being denied.
- Solution: Regularly review and update your team on insurance policies, payer guidelines, and common mistakes to watch out for. This will help you avoid claim rejection due to policy violations.
The Denial Management Process: What to Do When a Claim is Denied

Credit: resolvhealthcare.com
Despite your best efforts, some claims will inevitably be denied. The key is to have a clear and efficient denial management process in place. Here’s a simple step-by-step guide for handling denied claims:
Review the Denial Reason
-
Examine the reason code provided by the insurance company. This will give you an idea of why the claim was denied and what steps need to be taken to resolve it.
Appeal the Denial
-
If the denial is based on an incorrect reason, you can file an appeal. Provide additional documentation, correct errors, or offer clarification to support your case.
Resubmit the Claim
-
After making necessary corrections or submitting additional documentation, resubmit the claim for review. Keep track of the claim’s status to ensure timely payment.
Follow Up Regularly
-
Denial management is an ongoing process. Make sure to follow up with insurance companies until the claim is paid.
By creating an efficient denial management system and following the steps above, you can increase your chances of getting paid for services rendered.
The Bottom Line
Dealing with claim denials in medical billing can be frustrating, but you don’t have to handle it alone. At TMS Billing, we understand the ins and outs of the billing process and are here to help. From verifying eligibility to managing denials, we specialize in minimizing claim denials and improving your billing accuracy.
If you’re tired of dealing with rejected claims and want a smoother, more efficient process, we’re here to help. Let us take the stress out of billing so you can focus on what really matters.
FAQ’s
Here’s a look at some of your most asked queries.
What is a claim denial in medical billing?
A claim denial is when an insurance company refuses to pay for a medical service due to errors, eligibility issues, or missing information.
How can I reduce claim denials?
Improve eligibility verification, ensure accurate coding, use prior authorization, and stay updated on payer requirements.
What is the denial management process?
It involves reviewing denied claims, appealing them, correcting errors, and resubmitting for payment.
What role does coding play in claim denials?
Incorrect or mismatched codes can lead to denials. Accurate coding ensures proper claim processing.
What should I do if my claim is denied?
Review the denial reason, appeal, correct mistakes, and resubmit the claim. Follow up with the insurer.





